FAQ’s
Aesthetics
Dental Crowns
Discomfort or sensitivity. Your newly crowned tooth may be sensitive immediately after the procedure as the anesthesia begins to wear off. If the tooth that has been crowned still has a nerve in it, you may experience some heat and cold sensitivity. Your dentist may recommend that you brush your teeth with toothpaste designed for sensitive teeth.
Chipped crown . Crowns made of all porcelain can sometimes chip. If the chip is small, a composite resin can be used to repair the chip with the crown remaining in your mouth. If the chipping is extensive, the crown may need to be replaced.
Loose crown . Sometimes the cement washes out from under the crown. Not only does this allow the crown to become loose, it allows bacteria to leak in and cause decay to the tooth that remains. If your crown feels loose, contact our office or email us .
Crown falls off . If this happens, contact our office or email us immediately. Our dentists and staff can then give you specific instructions on how to care for your tooth and crown for the day or so until you can be seen for an evaluation. Your dentist may be able to re-cement your crown in place; if not, a new crown is required.
Allergic reaction . Because the metals used to make crowns are usually a mixture of metals, an allergic reaction to the metals or porcelain used in crowns can occur, but this is extremely rare. Please do kindly inform our staff on any allgeric reactions you may have before any medical or dental treatment.

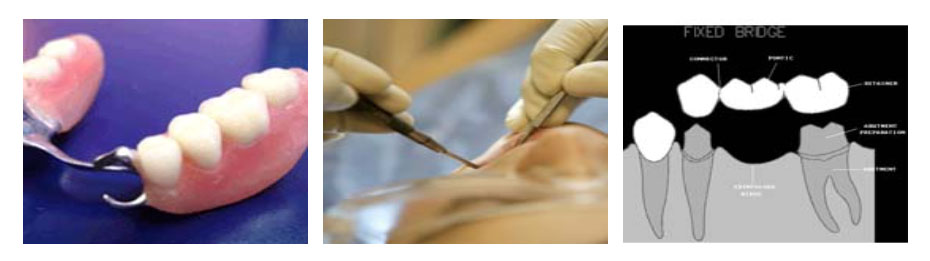
Dental Bridge
Dental Bonding
Advantages: Bonding is among the easiest and least expensive of cosmetic dental procedures. Unlike veneers and crowns, which are customized tooth coverings that must be manufactured in a laboratory, bonding usually can be done in one office visit unless several teeth are involved. Another advantage, compared with veneers and crowns, is that the least amount of tooth enamel is removed. Also, unless dental bonding is being performed to fill a cavity, anesthesia is usually not required.
Disadvantages : Although the material used in dental bonding is somewhat stain resistant, it does not resist stains as well as veneers and crowns. Another disadvantage is that the bonding materials do not last as long nor are as strong as other restorative procedures, such as crowns, veneers, or fillings. Additionally, bonding materials can chip and break off the tooth.
Because of some of the limitations of bonding, some dentists view bonding as best suited for small cosmetic changes, for temporary correction of cosmetic defects, and for correction of teeth in areas of very low bite pressure usually at the front teeth. Consult with your dentist about the best cosmetic approach for your particular problem.
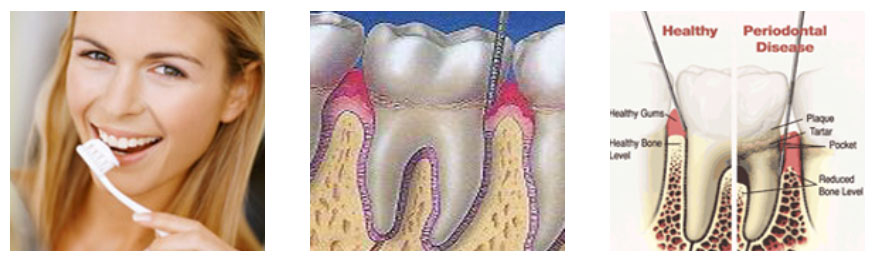
No. Simply follow good oral hygiene practices. Brush your teeth at least twice a day, floss at least once a day and see your dentist for regular professional check-ups and cleanings.
Because bonding material can chip, it is important to avoid such habits as biting fingernails; chewing on pens, ice or other hard food objects; or using your bonded teeth as an opener. If you do notice any sharp edges on a bonded tooth or if your tooth feels odd when you bite down, call your dentist.
Implants
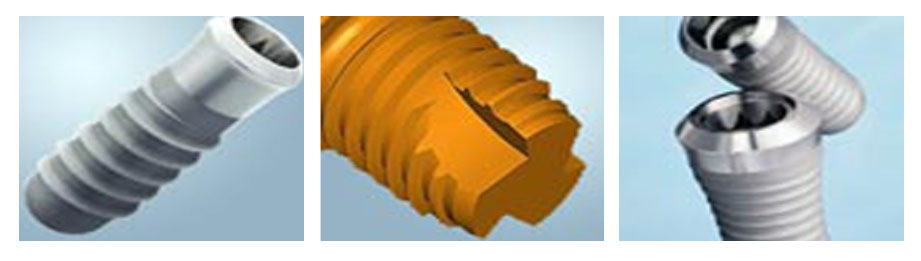
Anyone who is missing one or more (even all) of their teeth may be a candidate for implants.
If one or a few of the teeth are missing, implants in conjunction with a crown or bridge can replace those teeth and function as normal teeth without losing more bone and being subject to decay.
If all or most of your teeth are missing, then implants may be placed to anchor a loose denture. Sometimes, if there is already some bone loss, bone can be added and regenerated or a technique called bone expansion can be used to create a more ideal site for the implant(s). Ultimately, a consultation with a dentist who is knowledgeable on these procedures can help determine your individual needs.

When you lose your teeth, you gradually lose the bone that supported them. As this bone disappears, problems with other teeth nearby and a lack of support for dentures, partials and bridges increase. These could include pain, mobility, lack of retention for prosthetics, sharp, painful ridges, mobile gum tissue and sore spots.
The tongue enlarges to accommodate spaces of missing teeth. With tooth loss, a five-fold decrease in function occurs and the diet shifts to softer foods. Also, when bone is lost, numbness to the lower lip or even the possibility of fracture of the jaw rises.
Since the bone is deteriorating, it will spread and deteriorate around healthy teeth and ultimately cause the loss of those teeth similar to a domino effect.
This progression affects the ability to provide the same treatment in the later stages of bone loss than if treatment had been started earlier in the process. It's much better to replace a tooth BEFORE these side effects occur. A patient risks the possibility of not being able to provide the same, simple type of treatment that would have been possible earlier if treatment is delayed.
Orthodontics
Children and adults can both benefit from orthodontics, because healthy teeth can be moved at almost any age. Because monitoring growth and development is crucial to managing some orthodontic problems well, it is recommended that children have an orthodontic screening before the age of 7. Some orthodontic problems may be easier to correct if treated early. Waiting until all the permanent teeth have come in, or until facial growth is nearly complete, may make correction of some problems more difficult.
An orthodontic evaluation at any age is advisable if a parent, family dentist or the patient's physician has noted a problem.
Most malocclusions are inherited, but some are acquired. Inherited problems include crowding of teeth, too much space between teeth, extra or missing teeth, and a wide variety of other irregularities of the jaws, teeth and face.
Acquired malocclusions can be caused by trauma (accidents), thumb, finger or dummy (pacifier) sucking, airway obstruction by tonsils and adenoids, dental disease or premature loss of primary (baby) or permanent teeth. Whether inherited or acquired, many of these problems affect not only alignment of the teeth but also facial development and appearance as well.
In general, active treatment time with orthodontic appliances (braces) ranges from one to three years. Interceptive, or early treatment procedures, may take only a few months. The actual time depends on the growth of the patient's mouth and face, the cooperation of the patient and the severity of the problem. Mild problems usually require less time, and some individuals respond faster to treatment than others. Use of rubber bands and/or headgear, if prescribed by the orthodontist, contributes to completing treatment as scheduled.
While orthodontic treatment requires a time commitment, patients are rewarded with healthy teeth, proper jaw alignment and a beautiful smile that lasts a lifetime. Teeth and jaws in proper alignment look better, work better, contribute to general physical health and can improve self-confidence.

Brackets are the small squares that are bonded directly to each tooth with a special dental bonding agent or are attached to orthodontic bands. Brackets act like handles, holding the arch wires that move the teeth.
Orthodontic bands are stainless steel, clear or tooth-colored materials that are cemented with dental bonding agents or cement to teeth. They wrap around each tooth to provide an anchor for the brackets. The clear or tooth-colored bands are more cosmetically appealing options but are more expensive than stainless steel. They are not used in all patients. Some people have only brackets and no bands.
Spacers are separators that fit between teeth to create a small space prior to placement of orthodontic bands. Arch wires attach to the brackets and act as tracks to guide the movement of the teeth. Arch wires can be made of metal or be clear or tooth-colored.
Ties are small rubber rings or fine wires that fasten the arch wire to the brackets. They can be clear, metal or colored. A buccal tube on the band of the last molar holds the end of the arch wire securely in place.

Tiny elastic rubber bands , called ligatures, hold the arch wires to the brackets.
Springs may be placed on the arch wires between brackets to push, pull, open or close the spaces between teeth.
Two bands on the upper teeth may have headgear tubes on them to hold the facebow of the headgear in place.
Elastics or rubber bands attach to hooks on brackets and are worn between the upper and lower teeth in various ways. They apply pressure to move the upper teeth against the lower teeth to achieve a perfect fit of individual teeth.
Face bow headgear is the wire gadget that is used to move the upper molars back in the mouth to correct bite discrepancies and also to create room for crowded anterior teeth. The face bow consists of an inner metal part shaped like a horseshoe that goes in the mouth, attaching to buccal tubes, and an outer part that goes around the outside of the face and is connected to a headgear strap.

Pulling baby teeth may be necessary to allow severely crowded permanent teeth to come in at a normal time in a reasonably normal location. If the teeth are severely crowded, it may be clear that some uninterrupted permanent teeth (usually the canine teeth) will either remain impacted (teeth that should have come in, but have not), or come in to a highly undesirable position. To allow severely crowded teeth to move on their own into much more desirable positions, sequential removal of baby teeth and permanent teeth (usually first premolars) can dramatically improve a severe crowding problem. This sequential extraction of teeth, called serial extraction, is typically followed by comprehensive orthodontic treatment after tooth eruption has improved as much as it can on its own.
After all the permanent teeth have come in, the pulling of permanent teeth may be necessary to correct crowding or to make space for necessary tooth movement to correct a bite problem. Proper extraction of teeth during orthodontic treatment should leave the patient with both excellent functionand a pleasing look.
After your braces are taken off, your teeth will be thoroughly cleaned. Your orthodontist may want to take another set of x-rays and bite impressions to check how well the braces straightened your teeth and to see if any wisdom teeth have developed. If wisdom teeth are beginning to come in after your braces have been removed, your orthodontist may recommend the wisdom teeth be pulled to prevent your newly straightened teeth from shifting position in your mouth.
Your orthodontist will also fit you with a retainer. A retainer is a custom-made, removable appliance that help teeth to maintain their new position after braces have been removed. Retainers can also be used to treat minor orthodontic problems. The use of a retainer is a very important part of post-braces care. Retainers, which are typically made of rubber or clear plastic and metal wires that cover the outside surface of the teeth, need to be worn all the time for the first 6 months and then usually only during sleep. The time frame for wearing a retainer will vary from patient to patient. The reason why a retainer is needed is that even though braces may have successfully straightened your teeth, they are not completely settled in their new position until the bones, gums, and muscles adapt to the change. Also, after long periods of time, teeth tend to shift.
Headgear: This appliance applies pressure to the upper teeth and upper jaw to guide the rate and direction of upper jaw growth and upper tooth eruption. The headgear may be removed by the patient and is usually worn 10 to 12 hours per day.
Herbst: The Herbst appliance is usually fixed to the upper and lower molar teeth and may not be removed by the patient. By holding the lower jaw forward and influencing jaw growth and tooth positions, the Herbst appliance can help correct severe protrusion of the upper teeth.
Bionator: This removable appliance holds the lower jaw forward and guides eruption of the teeth into a more desirable bite while helping the upper and lower jaws to grow in proportion with each other. Patient compliance in wearing this appliance is essential for successful improvement.
Palatal Expansion Appliance: A child's upper jaw may also be too narrow for the upper teeth to fit properly with the lower teeth (a crossbite). When this occurs, a palatal expansion appliance can be fixed to the upper back teeth. This appliance can markedly expand the width of the upper jaw.
The decision about when and which of these or other appliances to use for orthopedic correction is based on each individual patient's problem. Usually one of several appliances can be used effectively to treat a given problem. Patient cooperation and the experience of the treating orthodontist are critical elements in success of dentofacial orthopedic treatment.
Prosthodontics
An orthodontic evaluation at any age is advisable if a parent, family dentist or the patient's physician has noted a problem.

You may have difficulty pronouncing certain words. If so, practice by saying the difficult wordsout loud. With practice and with time you will become accustomed to speaking properly with your denture.
If your dentures "click" while you're talking, you should contact your dentist. Your dentures may occasionally slip when you laugh, cough, or smile. Reposition the dentures by gently biting down and swallowing. If any speaking problem persists, consult your dentist or prosthodontist.
- Use the minimum amount necessary to provide the maximum benefit. Apply less than you think you need, and then gradually increase the amount until you feel comfortable.
- Distribute the adhesive evenly on the tissue bearing surface of the denture
- When oral hygiene practices cannot be sustained.
- Apply or reapply when necessary to provide the desired effect
- Always apply the adhesive to a thoroughly clean denture
- Remember adhesives work best with a well-fitting denture
Paste application
Apply to a dry or preferably wet denture. Avoid placing adhesive close to the denture borders. If the adhesive oozes, use less of the product. For dentures on the upper jaw, apply three short strips of adhesive-or s series of small dots-along the ridge area and one down the center. For dentures on the lower jaw, apply three short strips of adhesive-or s series of small dots-in the center of the ridge area.Powder application
Sprinkle a thin, uniform layer throughout the tissue-bearing surface of the denture. Shake off excess powder and press the denture into place. Powders may be preferred over pastes because they are easier to clean off the denture and tissue. In addition, they don't have the same tendency as pastes do to "shim" (keep the denture away from the tissue).Endodontics
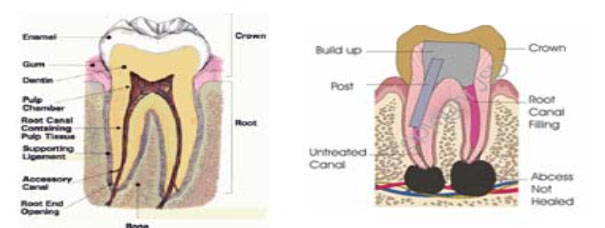
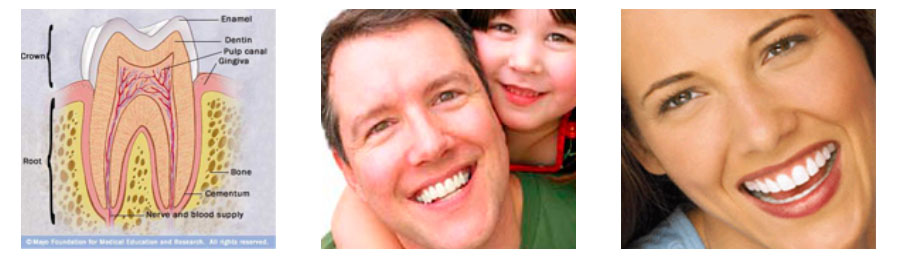
What is Endodontics? Endodontics deals with treatments like crowning/capping, inlays, outlays, root canal treatments and restorations
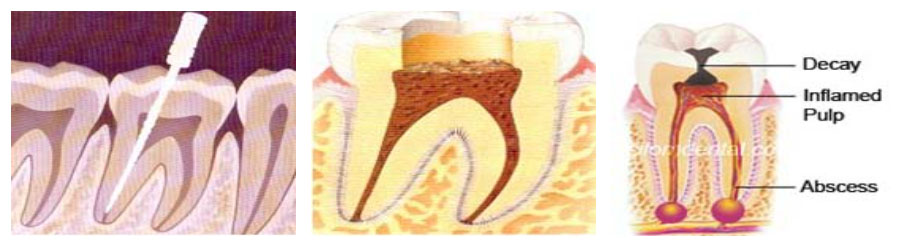
- Swelling that may spread to other areas of the face, neck, or head
- Bone loss around the tip of the root
- Drainage problems extending outward from the root. A hole can occur through the side of the tooth with drainage into the gums or through the cheek with drainage into the skin
- Sometimes no symptoms are present. However, signs to look for include:
- Severe toothache pain upon chewing or application of pressure
- Prolonged sensitivity/pain to heat or cold temperatures (after the hot or cold object has been removed)
- Discoloration (a darkening) of the tooth
- Swelling and tenderness in the nearby gums
- A persistent or recurring pimple on the gums
- More than the normally anticipated number of root canals in a tooth (leaving one of them uncleaned) An undetected crack in the root of a tooth
- Inadequate dental restoration
- A breakdown of the inner sealing material over time, allowing bacteria to recontaminate the inner aspects of the tooth
Saving your natural teeth is the very best option, if possible. Your natural teeth allow you to eat a wide variety of foods necessary to maintain proper nutrition. The root canal procedure is the treatment of choice.
The only alternative to a root canal procedure is having the tooth extracted and replaced with a bridge , implant , or removable partial denture to restore chewing function and prevent adjacent teeth from shifting.
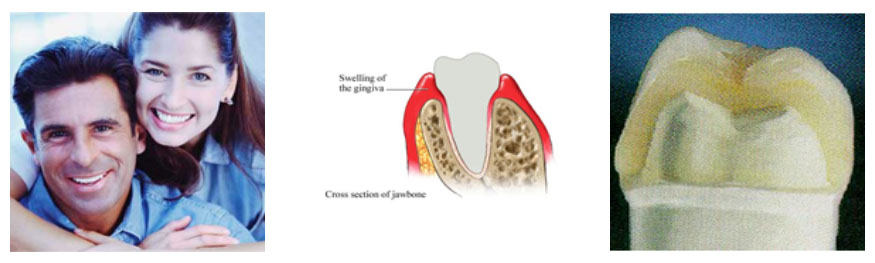
Periodontics
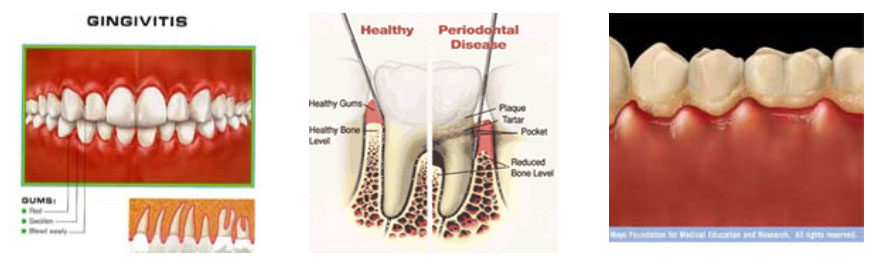 Periodontics deals with treatment of diseases of gum, surrounding teeth. The condition is treated by scaling, deep curettage, flap surgery, alveolar bone reconstruction surgery, bone grafting etc.
Periodontics deals with treatment of diseases of gum, surrounding teeth. The condition is treated by scaling, deep curettage, flap surgery, alveolar bone reconstruction surgery, bone grafting etc.Glossary

Abutment:
A tooth or teeth used to support and anchor a fixed bridge or removable denture prosthesis.
Alveolar Process (ridge):
The projection of bone that surrounds the roots of the teeth. The ridge is the remainder of the process after extractions.
Amalgam (silver filling):
A metal alloy consisting of silver, tin, zinc and copper combined with mercury and used as a restorative material in operative dentistry.
Analgesia:
Administration of a drug resulting in loss of pain sensation without the loss of consciousness.
Anterior teeth:
The front teeth. They include the six upper front teeth and six lower front teeth.

Bitewing x-ray:
A specific type of x-ray that shows, simultaneously, the crowns of upper and lower posterior teeth and a portion of their roots and supporting structures. Generally used to diagnose the presence of dental decay in adjoining tooth surfaces.
Bridge:
A replacement for one or more missing or extracted natural teeth, supported and held by attachments to restored teeth, and usually not removable. (Sometimes referred to as a fixed denture.) The cost of bridgework is usually calculated in units consisting of each crowned abutment tooth and each artificial tooth replacing a missing natural tooth (called a pontic).
Cap:
A layman's term for "jacket" (see "jacket" below). Caries: Decay in teeth. Cavities: Destruction of the tooth structure as a result of dental caries. Usually classified by the number of tooth surfaces affected. Cosmetic dentistry : Any dental service performed primarily to improve appearance. Crown:A fixed restoration covering the major part of the natural tooth, usually fabricated of gold, porcelain, or acrylic resin.
Deciduous:
The first teeth, ("baby teeth"). See "Primary Teeth" below.
Dental Arch:
The curved structure of the teeth or alveolar ridge. A horseshoe-like arrangement of the maxilla and mandible (upper and lower jaw).
Dentition:
Natural teeth in the dental arch. Natural teeth may be primary or secondary teeth.
Denture:
An artificial substitute for missing natural teeth and adjacent structures.
Complete Denture:
A dental prosthesis which replaces the lost natural teeth and associated structures of the entire upper or lower jaw.
Partial Denture:
An artificial replacement of one or more but less than all of the natural teeth and associated structures. Usually removable.
Endodontics:
The branch of dentistry concerned with the diagnosis and treatment of diseases of the pulp chamber and pulp canals.

